History of medicine
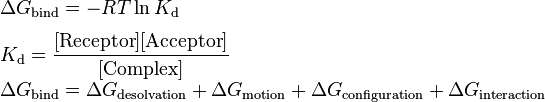
Prehistoric medicine:
There is no specific time that we can say when we used the plants for the first time in healing but the use of plants as healing agents is a long-standing practice. Over time through emulation of the behavior of animals, a medicinal knowledge base developed and was passed between generations. As
clannish culture specialized specific castes,
Shamans and
apothecaries performed the 'niche occupation' of healing.
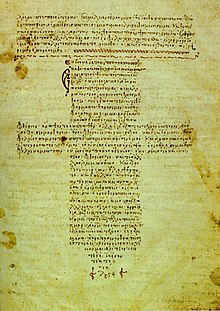
The Hippocratic Corpus, is a collection of early medical works from ancient Greece strongly associated with the ancient Greek physician Hippocrates and his teachings
Antiquity:
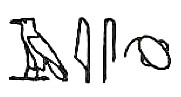
The Edwin Smith Surgical Papyrus, written in the 17th century BCE, contains the earliest recorded reference to the brain
Ancient Egypt developed a large, varied and fruitful medical tradition. Herodotus described the Egyptians as "the healthiest of all men, next to the Libyans", due to the dry climate and the notable public health system that they possessed. According to him, the practice of medicine is so specialized among them that each physician is a healer of one disease and no more." Although Egyptian medicine, to a good extent, dealt with the supernatural, it eventually developed a practical use in the fields of anatomy, public health, and clinical diagnostics.
Medical information in the Edwin Smith Papyrus may date to a time as early as 3000 BCE. The earliest known surgery was performed around 2750 BCE. Imhotep in the 3rd dynasty is sometimes credited with being the founder of ancient Egyptian medicine and with being the original author of the Edwin Smith Papyrus, detailing cures, ailments and anatomical observations. The Edwin Smith Papyrus is regarded as a copy of several earlier works and was written c. 1600 BCE. It is an ancient textbook on surgery almost completely devoid of magical thinking and describes in exquisite detail the examination, diagnosis, treatment, and prognosis of numerous ailments.
The Kahun Gynaecological Papyrus treats women's complaints, including problems with conception. Thirty four cases detailing diagnosis a treatment survive, some of them fragmentarily. Dating to 1800 BCE, it is the oldest surviving medical text of any kind.
Medical institutions, referred to as Houses of Life are known to have been established in ancient Egypt as early as the 1st Dynasty.
The earliest known physician is also credited to ancient Egypt: Hesy-Ra, “Chief of Dentists and Physicians” for King Djoser in the 27th century BCE.Also, the earliest known woman physician, Peseshet, practiced in Ancient Egypt at the time of the 4th dynasty. Her title was “Lady Overseer of the Lady Physicians.” In addition to her supervisory role, Peseshet trained midwives at an ancient Egyptian medical school in Sais.
The oldest Babylonian texts on medicine date back to the Old Babylonian period in the first half of the 2nd millennium BCE. The most extensive Babylonian medical text, however, is the Diagnostic Handbook written by the ummânū, or chief scholar, Esagil-kin-apli of Borsippa, during the reign of the Babylonian king Adad-apla-iddina (1069-1046 BCE).
Along with the Egyptians the Babylonians introduced the practice of diagnosis, prognosis, physical examination, and remedies. In addition, the Diagnostic Handbook introduced the methods of therapy and etiology. The text contains a list of medical symptoms and often detailed empirical observations along with logical rules used in combining observed symptoms on the body of a patient with its diagnosis and prognosis.
The Diagnostic Handbook was based on a logical set of axioms and assumptions, including the modern view that through the examination and inspection of the symptoms of a patient, it is possible to determine the patient's disease, its aetiology and future development, and the chances of the patient's recovery. The symptoms and diseases of a patient were treated through therapeutic means such as bandages, herbs and creams.
There was little development after the medieval era. Major European treatises on medicine took 200 years to reach the Middle East, where local rulers might consult Western doctors to get the latest treatments. Medical works in Arabic, Turkish, and Persian as late as 1800 were based on medieval Islamic medicine.
The Atharvaveda, a sacred text of Hinduism dating from the Early Iron Age, is the first Indian text dealing with medicine, like the medicine of the Ancient Near East based on concepts of the exorcism of demons and magic. The Atharvaveda also contain prescriptions of herbs for various ailments. The use of herbs to treat ailments would later form a large part of Ayurveda.
In the first millennium BCE, there emerges in post-Vedic India the traditional medicine system known as Ayurveda, meaning the "complete knowledge for long life". Its two most famous texts belong to the schools of Charaka, born c. 600 BCE, and Sushruta, born 600 BCE. While these writings display some limited continuities with the earlier medical ideas known from the Vedas, historians have been able to demonstrate direct historical connections between early Ayurveda and the early literature of the Buddhists and Jains. The earliest foundations of Ayurveda were built on a synthesis of traditional herbal practices together with a massive addition of theoretical conceptualizations, new nosologies and new therapies dating from about 400 BCE onwards, and coming out of the communities of thinkers who included the Buddha and others.
According to the compendium of Charaka, the Charakasamhitā, health and disease are not predetermined and life may be prolonged by human effort. The compendium of Suśruta, the Suśrutasamhitā defines the purpose of medicine to cure the diseases of the sick, protect the healthy, and to prolong life. Both these ancient compendia include details of the examination, diagnosis, treatment, and prognosis of numerous ailments. The Suśrutasamhitā is notable for describing procedures on various forms of surgery, including rhinoplasty, the repair of torn ear lobes, perineal lithotomy, cataract surgery, and several other excisions and other surgical procedures. Most remarkable is Sushruta's penchant for scientific classification: His medical treatise consists of 184 chapters, 1,120 conditions are listed, including injuries and illnesses relating to ageing and mental illness. The Sushruta Samhita describe 125 surgical instrument, 300 surgical procedures and classifies human surgery in 8 categories
The Ayurvedic classics mention eight branches of medicine: kāyācikitsā (internal medicine), śalyacikitsā (surgery including anatomy), śālākyacikitsā (eye, ear, nose, and throat diseases), kaumārabhṛtya (pediatrics), bhūtavidyā (spirit medicine), and agada tantra (toxicology), rasāyana (science of rejuvenation), and vājīkaraṇa (aphrodisiacs, mainly for men). Apart from learning these, the student of Āyurveda was expected to know ten arts that were indispensable in the preparation and application of his medicines: distillation, operative skills, cooking, horticulture, metallurgy, sugar manufacture, pharmacy, analysis and separation of minerals, compounding of metals, and preparation of alkalis. The teaching of various subjects was done during the instruction of relevant clinical subjects. For example, teaching of anatomy was a part of the teaching of surgery, embryology was a part of training in pediatrics and obstetrics, and the knowledge of physiology and pathology was interwoven in the teaching of all the clinical disciplines. The normal length of the student's training appears to have been seven years. But the physician was to continue to learn.
As an alternative form of medicine in India, Unani medicine got deep roots and royal patronage during medieval times. It progressed during Indian sultanate and mughal periods. Unani medicine is very close to Ayurveda. Both are based on theory of the presence of the elements (in Unani, they are considered to be fire, water, earth and air) in the human body. According to followers of Unani medicine, these elements are present in different fluids and their balance leads to health and their imbalance leads to illness.
By the 18th century A.D., Sanskrit medical wisdom still dominated. Muslim rulers built large hospitals in 1595 in Hyderabad, and in Delhi in 1719, and numerous commentaries on ancient texts were written. Some European plants and medicinals were gradually incorporated into the Indian pharmacopeia, but otherwise there was little intellectual exchange with the West.
China also developed a large body of traditional medicine. Much of the philosophy of traditional Chinese medicine derived from empirical observations of disease and illness by Taoist physicians and reflects the classical Chinese belief that individual human experiences express causative principles effective in the environment at all scales. These causative principles, whether material, essential, or mystical, correlate as the expression of the natural order of the universe.
The foundational text of Chinese medicine is the Huangdi neijing, or Yellow Emperor's Inner Canon, written 5th century to 3rd century BCE). near the end of the 2nd century AD, during the Han dynasty, Zhang Zhongjing, wrote a Treatise on Cold Damage, which contains the earliest known reference to the Neijing Suwen. The Jin Dynasty practitioner and advocate of acupuncture and moxibustion, Huangfu Mi (215-282), also quotes the Yellow Emperor in his Jiayi jing, c. 265. During the Tang Dynasty, the Suwen was expanded and revised, and is now the best extant representation of the foundational roots of traditional Chinese medicine. Traditional Chinese Medicine that is based on the use of herbal medicine, acupuncture, massage and other forms of therapy has been practiced in China for thousands of years.
In the 18th century, during the Qing dynasty, there was a proliferation of popular books as well as more advanced encyclopedias on traditional medicine. Jesuit missionaries introduced Western science and medicine to the royal court, the Chinese physicians ignored them.
Finally in the 19th century, Western medicine was introduced at the local level by Christian medical missionaries from the London Missionary Society (Britain), the Methodist Church (Britain) and the Presbyterian Church (USA). Benjamin Hobson (1816-1873) in 1839, set up a highly successful Wai Ai Clinic in Guangzhou, China. The Hong Kong College of Medicine for Chinese was founded in 1887 by the London Missionary Society, with its first graduate (in 1892) being Sun Yat-sen, who later led the Chinese Revolution (1911). The Hong Kong College of Medicine for Chinese was the forerunner of the School of Medicine of the University of Hong Kong, which started in 1911.
Due to the social custom that men and women should not be near to one another, the women of China were reluctant to be treated by male doctors. The missionaries sent women doctors such as Dr. Mary H. Fulton (1854-1927). Supported by the Foreign Missions Board of the Presbyterian Church (USA) she in 1902 founded the first medical college for women in China, the Hackett Medical College for Women, in Guangzhou.
Greek and Roman medicine:
Around 800 BCE Homer in The Iliad gives descriptions of wound treatment by "the two sons of Asklepios, the admirable physicians Podaleirius and Machaon and one acting doctor, Patroclus. Because Machaon is wounded and Podaleirius is in combat Eurypylus asks Patroclus “to cut out this arrow from my thigh, wash off the blood with warm water and spread soothing ointment on the wound." Askelpios like Imhotep becomes god of healing over time. Temples dedicated to the healer-god Asclepius, known as Asclepieia (Ancient Greek: Ἀσκληπιεῖα, sing. Ἀσκληπιεῖον, 'Asclepieion), functioned as centers of medical advice, prognosis, and healing. At these shrines, patients would enter a dream-like state of induced sleep known as enkoimesis (ἐγκοίμησις) not unlike anesthesia, in which they either received guidance from the deity in a dream or were cured by surgery. Asclepeia provided carefully controlled spaces conducive to healing and fulfilled several of the requirements of institutions created for healing. In the Asclepieion of Epidaurus, three large marble boards dated to 350 BCE preserve the names, case histories, complaints, and cures of about 70 patients who came to the temple with a problem and shed it there. Some of the surgical cures listed, such as the opening of an abdominal abscess or the removal of traumatic foreign material, are realistic enough to have taken place, but with the patient in a state of enkoimesis induced with the help of soporific substances such as opium.
The first known Greek medical school opened in Cnidus in 700 BCE. Alcmaeon, author of the first anatomical work, worked at this school, and it was here that the practice of observing patients was established. As was the case elsewhere, the ancient Greeks developed a humoral medicine system where treatment sought to restore the balance of humours within the body.
A towering figure in the history of medicine was the physician Hippocrates of Kos (c. 460 – c. 370 BCE), considered the "father of modern medicine." The Hippocratic Corpus is a collection of around seventy early medical works from ancient Greece strongly associated with Hippocrates and his students. Most famously, Hippocrates invented the Hippocratic Oath for physicians, which is still relevant and in use today.
Hippocrates and his followers were first to describe many diseases and medical conditions. He is given credit for the first description of clubbing of the fingers, an important diagnostic sign in chronic suppurative lung disease, lung cancer and cyanotic heart disease. For this reason, clubbed fingers are sometimes referred to as "Hippocratic fingers".
Hippocrates was also the first physician to describe Hippocratic face in Prognosis. Shakespeare famously alludes to this description when writing of Falstaff's death in Act II, Scene iii. of Henry V. Hippocrates began to categorize illnesses as acute, chronic, endemic and epidemic, and use terms such as, "exacerbation, relapse, resolution, crisis, paroxysm, peak, and convalescence."
Another of Hippocrates's major contributions may be found in his descriptions of the symptomatology, physical findings, surgical treatment and prognosis of thoracic empyema, i.e. suppuration of the lining of the chest cavity. His teachings remain relevant to present-day students of pulmonary medicine and surgery. Hippocrates was the first documented chest surgeon and his findings are still valid.
View of the Askleipion of Kos, the best preserved instance of an Asklepieion
The Plinthios Brokhos as described by Greek physician Heraklas, a sling for binding a fractured jaw. These writings were preserved in one of Oribasius' collections
Two great Alexandrians laid the foundations for the scientific study of anatomy and physiology, Herophilus of Chalcedon and Erasistratus of Ceos. Other Alexandrian surgeons gave us; ligature (hemostasis), lithotomy, hernia operations, ophthalmic surgery, plastic surgery, methods of reduction of dislocations and fractures,tracheotomy, and mandrake as anesthesia. Most of what we know of them comes from Celsus and Galen of Pergamum (Greek: Γαληνός)
Herophilus of Chalcedon, working at the medical school of Alexandria placed intelligence in the brain, and connected the nervous system to motion and sensation. Herophilus also distinguished between veins and arteries, noting that the latter pulse while the former do not. He and his contemporary, Erasistratus of Chios, researched the role of veins and nerves, mapping their courses across the body. Erasistratus connected the increased complexity of the surface of the human brain compared to other animals to its superior intelligence. He sometimes employed experiments to further his research, at one time repeatedly weighing a caged bird, and noting its weight loss between feeding times. In Erasistratus' physiology, air enters the body, is then drawn by the lungs into the heart, where it is transformed into vital spirit, and is then pumped by the arteries throughout the body. Some of this vital spirit reaches the brain, where it is transformed into animal spirit, which is then distributed by the nerves.
The Greek Galen was one of the greatest surgeons of the ancient world and performed many audacious operations—including brain and eye surgeries— that were not tried again for almost two millennia. Later, in medieval Europe, Galen's writings on anatomy became the mainstay of the medieval physician's university curriculum along; but they suffered greatly from stasis and intellectual stagnation. In the 1530s, however, Belgian anatomist and physician Andreas Vesalius took on a project to translate many of Galen's Greek texts into Latin. Vesalius's most famous work, De humani corporis fabrica, was greatly influenced by Galenic writing and form. The works of Galen were regarded as authoritative until well into the Middle Ages.
The Romans invented numerous surgical instruments, including the first instruments unique to women, as well as the surgical uses of forceps, scalpels, cautery, cross-bladed scissors, the surgical needle, the sound, and speculas. Romans also performed cataract surgery.
- Islamic Middle Ages 9th-12th:
An Arabic manuscript, dated 1200, titled Anatomy of the Eye, authored by al-Mutadibih
The Islamic civilization rose to primacy in medical science as its physicians contributed significantly to the field of medicine, including anatomy, ophthalmology, pharmacology, pharmacy, physiology, surgery, and the pharmaceutical sciences. The Arabs were influenced by, and further developed Greek, Roman and Byzantine medical practices. Galen & Hippocrates were pre-eminent authorities.The translation of 129 works of ancient Greek physician Galen into Arabic by Hunayn ibn Ishaq and his assistants, and in particular Galen's insistence on a rational systematic approach to medicine, set the template for Islamic medicine, which rapidly spread throughout the Arab Empire. Muslim physicians set up dedicated hospitals.
- Medieval Europe 400 to 1400 AD:
A miniature depicting the Schola Medica Salernitana
After 400 A.D., most of the medical institutions of the Roman Empire broke down and disappeared. Medical services were provided, especially for the poor, in the thousands of monasteries that sprang up across Europe. Rich nobles gave permanent endowments to the monasteries, in the expectation that these good works would lead to their salvation, and lessen their time in purgatory. Catholic theology held that the sick, especially the poor peasants, would also gain grace and lessen their own time in purgatory, through their suffering. Most of the medical advances of the Roman empire were forgotten, at his medicine relied increasingly on folk remedies.
Wallis identifies a prestige hierarchy with university educated physicians on top, followed by learned surgeons; craft-trained surgeons; barber surgeons; itinernant specialists such as dentist and oculists; empirics; and midwives.
1) Schools:
The first medical schools were opened, most notably the Schola Medica Salernitana at Salerno in southern Italy. The cosmopolitan influences from Greek, Latin, Arabic, and Hebrew sources gave it an international reputation as the Hippocratic City. Students from wealthy families came for three years of preliminary studies and five of medical studies. Graduates were awarded the degree of "magister" (Latin for doctor); indeed physicians were 1st called "doctor" at Salerno. By the thirteenth century the medical school at Montpellier began to eclipse the Salernitan school. In the 12th century universities were founded in Italy, France and England which soon developed schools of medicine. The University of Montpellier in France and Italy's University of Padua and University of Bologna were leading schools. Nearly all the learning was from lectures and readings in Hippocrates, Galen, Avicenna and Aristotle. There was little clinical work or dissection.
2) Humours:
13th century illustration showing the veins
The underlying principle of most medieval medicine was Galen's theory of humours. This was derived from the ancient medical works, and dominated all western medicine until the 19th century. The theory stated that within every individual there were four humours, or principal fluids - black bile, yellow bile, phlegm, and blood, these were produced by various organs in the body, and they had to be in balance for a person to remain healthy. Too much phlegm in the body, for example, caused lung problems; and the body tried to cough up the phlegm to restore a balance. The balance of humours in humans could be achieved by diet, medicines, and by blood-letting, using leeches. The four humours were also associated with the four seasons, black bile-autumn, yellow bile-summer, phlegm-winter and blood-spring.
Healing included both physical and spiritual therapeutics, such as the right herbs, a suitable, diet, clean bedding, and the sense that care was always at hand. Other procedures used to help patients included the Mass, prayers, relics of saints, and music used to calm a troubled mind or quickened pulse.
Renaissance to Early Modern period 16th-18th century:
The Renaissance brought an intense focus on scholarship to Christian Europe. A major effort to translate the Arabic and Greek scientific works into Latin emerged. Europeans gradually became experts not only the ancient writings of the Romans and Greeks, but in the contemporary writings of Islamic scientists. During the later centuries of the Renaissance came an increase in experimental investigation, particularly in the field of dissection and body examination, thus advancing our knowledge of human anatomy.
The development of modern neurology began in the 16th century with Vesalius, who described the anatomy of the brain and other organs; he had little knowledge of the brain's function, thinking that it resided mainly in the ventricles. Over his lifetime he corrected over 200 of Galen's mistakes. Understanding of medical sciences and diagnosis improved, but with little direct benefit to health care. Few effective drugs existed, beyond opium and quinine. Folklore cures and potentially poisonous metal-based compounds were popular treatments. Independently from Ibn al-Nafis, Michael Servetus rediscovered the pulmonary circulation, but this discovery did not reach the public cause it was written down for the first time in the "Manuscript of Paris" in 1546, and later published in the theological work which he paid with his life in 1553. Later this was perfected by Renaldus Columbus and Andrea Cesalpino. Later William Harvey provided a refined and complete description of the circulatory system. The most useful tomes in medicine used both by students and expert physicians were Materia Medica and Pharmacopoeia.
Paracelsus (1493-1541), was an erratic and abusive innovator who rejected Galen and bookish knowledge, calling for experimental research, with heavy doses of mysticism, alchemy and magic mixed in. The point is that he rejected sacred magic (miracles) under Church auspisces and looked for cures in nature. He preached but he also pioneered the use of chemicals and minerals in medicine. His hermetical views were that sickness and health in the body relied on the harmony of man (microcosm) and Nature (macrocosm). He took an approach different from those before him, using this analogy not in the manner of soul-purification but in the manner that humans must have certain balances of minerals in their bodies, and that certain illnesses of the body had chemical remedies that could cure them. Most of his influence came after his death. Paracelsus is a highly controversial figure in the history of medicine, with most experts hailing him as a Father of Modern Medicine for shaking off religious orthodoxy and inspiring many researchers; others say he was a mystic more than a scientist and downplay his importance.
Vesalius's Fabrica contained many intricately detailed drawings of human dissections, often in allegorical poses
University training of physicians began in the 13th century.
The University of Padua began teaching medicine in 1222. It played a leading role in the identification and treatment of diseases and ailments, specializing in autopsies and the inner workings of the body. Starting in 1595, Padua's famous anatomical theatre drew artists and scientists studying the human body during public dissections. The intensive study of Galen led to critiques of Galen modeled on his own writing, as in the first book of Vesalius's De humani corporis fabrica. Andreas Vesalius held the chair of Surgery and Anatomy (explicator chirurgiae) and in 1543 published his anatomical discoveries in De Humani Corporis Fabrica. He portrayed the human body as an interdependent system of organ groupings. The book triggered great public interest in dissections and caused many other European cities to establish anatomical theatres.
At the University of Bologna the training of physicians began in 1219. The Italian city attracted students from across Europe. Taddeo Alderotti built a tradition of medical education that established the characteristic features of Italian learned medicine and was copied by medical schools elsewhere. Turisanus (d. 1320) was his student. The curriculum was revised and strengthened in 1560-1590. A representative professor was Julius Caesar Aranzi (Arantius) (1530–89). He became Professor of Anatomy and Surgery at the University of Bologna in 1556, where he established anatomy as a major branch of medicine for the first time. Aranzi combined anatomy with a description of pathological processes, based largely on his own research, Galen, and the work of his contemporary Italians. Aranzi discovered the 'Nodules of Aranzio' in the semilunar valves of the heart and wrote the first description of the superior levator palpebral and the coracobrachialis muscles. His books (in Latin) covered surgical techniques for many conditions, including hydrocephalus, nasal polyp, goitre and tumours to phimosis, ascites, haemorrhoids, anal abscess and fistulae.
Catholic women played large roles in health and healing in medieval and early modern Europe. A life as a nun was a prestigious role; wealthy families provided dowries for their daughters, and these funded the convents, while the nuns provided free nursing care for the poor.
The Catholic elites provided hospital services because of their theology of salvation that good works were the route to heaven. The Protestant reformers rejected the notion that rich men could gain God's grace through good works-and thereby escape purgatory-by providing cash endowments to charitable institutions. They also rejected the Catholic idea that the poor patients earned grace and salvation through their suffering. Protestants generally closed all the convents and most of the hospitals, sending women home to become housewives, often against their will. On the other hand, local officials recognized the public value of hospitals, and some were continued in Protestant lands, but without monks or nuns and in the control of local governments.
In London, the crown allowed two hospitals to continue their charitable work, under nonreligious control of city officials.The convents were all shut down but Harkness finds that women-some of them former nuns-were part of a new system that delivered essential medical services to people outside their family. The were employed by parishes and hospitals, as well as by private families, and provided nursing care as well as some medical, pharmaceutical, and surgical services.
Meanwhile, in Catholic lands such as France, rich families continued to fund convents and monasteries, and enrolled their daughters as nuns who provided free health services to the poor. Nursing was a religious role for the nurse, and there was little call for science.
During the Age of Enlightenment, the 18th-century, science was held in high esteem and physicians upgraded their social status by becoming more scientific. The health field was crowded with self-trained barber-surgeons, apothecaries, midwives, drug peddlers, and charlatans.
Across Europe medical schools relied primarily on lectures and readings. In the final year student would have limited clinical experience by trailing the professor through the wards. Laboratory work was uncommon, and dissections were rarely done because of legal restrictions on cadavers. Most schools were small, and only Edinburgh, Scotland, with 11,000 alumni, produced large numbers of graduates.
In Britain, there but three small hospitals after 1550. Pelling and Webster estimate that in London in the 1580 to 1600 period, out of a population of nearly 200,000 people, there were about 500 medical practitioners. Nurses and midwives are not included. There were about 50 physicians, 100 licensed surgeons, 100 apothecaries, and 250 additional unlicensed practitioners. In the last category about 25% were women. All across Britain-and indeed all of the world-the vast majority of the people in city, town or countryside depended for medical care on local amateurs with no professional training but with a reputation as wise healers who could diagnose problems and advise sick people what to do—and perhaps set broken bones, pull a tooth, give some traditional herbs or brews or perform a little magic to cure what ailed them.
The London Dispensary opened in 1696, the first clinic in the British Empire to dispense medicines to poor sick people. The innovation was slow to catch on, but new dispensaries were open in the 1770s. In the colonies, small hospitals opened in Philadelphia in 1752, New York in 1771, and Boston (Massachusetts General Hospital) in 1811.
Guy's Hospital 1820
Guy's Hospital, the first great British hospital opened in 1721 in London, with funding from businessman Thomas Guy. In 1821 a bequest of £200,000 by William Hunt in 1829 funded expansion for an additional hundred beds. Samuel Sharp (1709–78), a surgeon at Guy's Hospital, from 1733 to 1757, was internationally famous; his A Treatise on the Operations of Surgery (1st ed., 1739), was the first British study focused exclusively on operative technique.
English physician Thomas Percival (1740-1804) wrote a comprehensive system of medical conduct, Medical Ethics, or a Code of Institutes and Precepts, Adapted to the Professional Conduct of Physicians and Surgeons (1803) that set the standard for many textbooks.
19th century: Rise of modern medicine:
Anatomy of the heart (1890) by Enrique Simonet
The practice of medicine changed in the face of rapid advances in science, as well as new approaches by physicians. Hospital doctors began much more systematic analysis of patients' symptoms in diagnosis. Among the more powerful new techniques were anaesthesia, and the development of both antiseptic and aseptic operating theatres. Actual cures were developed for certain endemic infectious diseases. However the decline in many of the most lethal diseases was more due to improvements in public health and nutrition than to medicine. It was not until the 20th century that the application of the scientific method to medical research began to produce multiple important developments in medicine, with great advances in pharmacology and surgery.
Medicine was revolutionized in the 19th century and beyond by advances in chemistry and laboratory techniques and equipment, old ideas of infectious disease epidemiology were replaced with bacteriology and virology. Bacteria and microorganisms were first observed with a microscope by Antonie van Leeuwenhoek in 1676, initiating the scientific field microbiology.
In Vienna Ignaz Semmelweis (1818–1865) in 1847 dramatically reduced the death rate of new mothers from childbed fever by the simple expedient of requiring physicians to clean their hands before attending to women in childbirth. His discovery pre-dated the germ theory of disease. However, his discoveries were not appreciated by his contemporaries and came into general use only with discoveries of British surgeon Joseph Lister, who in 1865 proved the principles of antisepsis in the treatment of wound.
Louis Pasteur, by laboratory work that linked microorganisms with disease, brought about a revolution in medicine; he successfully reached out to instruct the educated classes of France in the importance of the germ theory. Pasteur with Claude Bernard (1813–1878) invented the process of pasteurization still in use today. Pasteur, along with Robert Koch founded bacteriology. Koch, who was awarded the Nobel Prize in 1905, became famous for the discovery of the tubercle bacillus (1882) and the cholera bacillus (1883) and for his development of Koch's postulates.
The quality of military medicine differed sharply among nations. A comparison of British and French surgical work on wounded sailors at the Battle of Trafalgar of 1805 shows that Royal Navy surgeons practiced triage, amputated immediately rather than delay the operation, and kept surgical areas clean. They were well trained and practiced up-to-date methods of surgery and hygiene. By contrast, French surgeons tolerated unhygienic facilities and had less training and skill, resulting in much higher mortality rates for their patients.
1) Women as nurses:
Women had always served in ancillary roles, and as midwives and healers. The professionalization of medicine forced them increasingly to the sidelines. As hospitals multiplied they relied in Europe on orders of Roman Catholic nun-nurses, and German Protestant and Anglican deaconesses in the early 19th century. They were trained in traditional methods of physical care that involved little knowledge of medicine. The breakthrough to professionalization based on knowledge of advanced medicine was led by Florence Nightingale in England.
She resolved to provide more advanced training than she saw on the Continent. At Kaiserswerth, where the first German nursing schools was founded in 1836 by Theodor Fliedner, she said, "The nursing was nil and the hygiene horrible.") Britain's male doctors preferred the old system, but Nightingale won out and her Nightingale Training School opened in 1860 and became a model. The Nightingale solution depended on the patronage of upper class women, and they proved eager to serve. Royalty became involved. In 1902 the wife of the British king took control of the nursing unit of the British army, became its president, and renamed it after herself as the Queen Alexandra's Royal Army Nursing Corps; when she died the next queen became president.
Today its Colonel In Chief is the daughter-in-law of Queen Elizabeth. In the United States, upper middle class women who already supported hospitals promoted nursing. The new profession proved highly attractive to women of all backgrounds, and schools of nursing opened in the late 19th century. They soon a function of large hospitals, where they provided a steady stream of low-paid idealistic workers. The International Red Cross began operations in numerous countries in the late 19th century, promoting nursing as an ideal profession for middle class women.
The Nightingale model was widely copied. Linda Richards (1841 – 1930) studied in London and became the professionally trained American nurse. She established nursing training programs in the United States and Japan, and created the first system for keeping individual medical records for hospitalized patients. The Russian Orthodox Church sponsored seven orders of nursing sisters in the late 19th century. They ran hospitals, clinics, almshouses, pharmacies, and shelters as well as training schools for nurses. In the Soviet era (1917-1991), with the aristocratic sponsors gone, nursing became a low-prestige occupation based in poorly maintained hospitals.
2) Women as doctors:
It was very difficult for women to become doctors before the 1970s. Elizabeth Blackwell (1821–1910) became the first woman to formally study and practice medicine in the United States. She was a leader in women's medical education. While Blackwell viewed medicine as a means for social and moral reform, her student Mary Putnam Jacobi (1842-1906) focused on curing disease. At a deeper level of disagreement, Blackwell felt that women would succeed in medicine because of their humane female values, but Jacobi believed that women should participate as the equals of men in all medical specialties using identical methods, values and insights.
Paris and Vienna were the two leading medical centers on the Continent in the era 1750-1914.
In 1770s-1850s Paris became a world center of medical research and teaching. The "Paris School" emphasized that teaching and research should be based in large hospitals and promoted the professionalization of the medical profession and the emphasis on sanitation and public health. A major reformer was Jean-Antoine Chaptal (1756-1832), a physician who was Minister of Internal Affairs. He created the Paris Hospital, health councils, and other bodies.
Louis Pasteur (1822-1895) was one of the most important founders of medical microbiology. He is remembered for his remarkable breakthroughs in the causes and preventions of diseases. His discoveries reduced mortality from puerperal fever, and he created the first vaccines for rabies and anthrax. His experiments supported the germ theory of disease. He was best known to the general public for inventing a method to treat milk and wine in order to prevent it from causing sickness, a process that came to be called pasteurization. He is regarded as one of the three main founders of microbiology, together with Ferdinand Cohn and Robert Koch. He worked chiefly in Paris and in 1887 founded the Pasteur Institute there to perpetuate his commitment to basic research and its practical applications. As soon as his institute was created, Pasteur brought together scientists with various specialties.
The first five departments were directed by Emile Duclaux (general microbiology research) and Charles Chamberland (microbe research applied to hygiene), as well as a biologist, Ilya Ilyich Mechnikov (morphological microbe research) and two physicians, Jacques-Joseph Grancher (rabies) and Emile Roux (technical microbe research). One year after the inauguration of the Institut Pasteur, Roux set up the first course of microbiology ever taught in the world, then entitled Cours de Microbie Technique (Course of microbe research techniques). It became the model for numeous research centers around the world named "Pasteur Institutes."
The First Viennese School of Medicine, 1750-1800, was led by the Dutchman Gerard van Swieten (1700-1772), who aimed to put medicine on new scientific foundations - promoting unprejudiced clinical observation, botanical and chemical research, and introducing simple but powerful remedies. When the Vienna General Hospital opened in 1784, it at once became the world's largest hospital and physicians acquired a facility that gradually developed into the most important research centre. Progress ended with the Napoleonic wars and the government shutdown in 1819 of all liberal journals and schools; this caused a general return to traditionalism and eclecticism in medicine.
Vienna was the capital of a diverse empire and attracted not just Germans but Czechs, Hungarians, Jews, Poles and others to its world-class medical facilities. After 1820 the Second Viennese School of Medicine emerged with the contributions of physicians such as Carl Freiherr von Rokitansky, Josef Škoda, Ferdinand Ritter von Hebra, and Ignaz Philipp Semmelweis. Basic medical science expanded and specialization advanced. Furthermore, the first dermatology, eye, as well as ear, nose, and throat clinics in the world were founded in Vienna. The textbook of ophthalmologist Georg Joseph Beer (1763-1821) Lehre von den Augenkrankheiten combined practical research and philosophical speculations, and became the standard reference work for decades.
After 1871 Berlin, the capital of the new German Empire, became a leading center for medical research. Robert Koch (1843-1910) was a representative leader. He became famous for isolating Bacillus anthracis (1877), the Tuberculosis bacillus (1882) and Vibrio cholerae (1883) and for his development of Koch's postulates. He was awarded the Nobel Prize in Physiology or Medicine in 1905 for his tuberculosis findings. Koch is one of the founders of microbiology, inspiring such major figures as Paul Ehrlich and Gerhard Domagk.
In the American Civil War (1861–65), as was typical of the 19th century, more soldiers died of disease than in battle, and even larger numbers were temporarily incapacitated by wounds, disease and accidents. Conditions were poor in the Confederacy, where doctors and medical supplies were in short supply.The war had a dramatic long-term impact on American medicine, from surgerical technique to hospitals to nursing and to research facilities.
The hygiene of the training and field camps was poor, especially at the beginning of the war when men who had seldom been far from home were brought together for training with thousands of strangers. First came epidemics of the childhood diseases of chicken pox, mumps, whooping cough, and, especially, measles. Operations in the South meant a dangerous and new disease environment, bringing diarrhea, dysentery, typhoid fever, and malaria. There were no antibiotics, so the surgeons prescribed coffee, whiskey, and quinine. Harsh weather, bad water, inadequate shelter in winter quarters, poor policing of camps, and dirty camp hospitals took their toll.
This was a common scenario in wars from time immemorial, and conditions faced by the Confederate army were even worse. The Union responded by building army hospitals in every state. What was different in the Union was the emergence of skilled, well-funded medical organizers who took proactive action, especially in the much enlarged United States Army Medical Department, and the United States Sanitary Commission, a new private agency. Numerous other new agencies also targeted the medical and morale needs of soldiers, including the United States Christian Commission as well as smaller private agencies.
The U.S. Army learned many lessons and in 1886, it established the Hospital Corps.
"Diagram of the causes of mortality in the army in the East" by Florence Nightingale
A major breakthrough in epidemiology came with the introduction of statistical maps and graphs. They allowed careful analysis of seasonality issues in disease incidents, and the maps allowed public health officials to identifical critical loci for the dissemination of disease. John Snow in London developed the methods. English nurse Florence Nightingale pioneered analysis of large amounts of statistical data, using graphs and tables, regarding the condition of thousands of patients in the Crimean War to evaluate the efficacy of hospital services. Her methods proved convincing and led to reforms in military and civilian hospitals, usually with the full support of the government.
By the late 19th and early 20th century English statisticians led by Francis Galton, Karl Pearson and Ronald Fisher developed the mathematical tools such as correlations and hypothesis tests that made possible much more sophisticated analysis of statistical data.
During the U.S. Civil War the Sanitary Commission collected enormous amounts of statistical data, and opened up the problems of storing information for fast access and mechanically searching for data patterns. The pioneer was John Shaw Billings (1838-1913). A senior surgeon in the war, Billings built the Library of the Surgeon General's Office (now the National Library of Medicine, the centerpiece of modern medical information systems. Billings figured out how to mechanically analyze medical and demographic data by turning facts into numbers and punching the numbers onto cardboard cards that could be sorted and counted by machine. The applications were developed by his assistant Herman Hollerith; Hollerith invented the punch card and counter-sorter system that dominated statistical data manipulation until the 1970s. Hollerith's company became International Business Machines (IBM) in 1911.
Japan:
European ideas of modern medicine were spread widely through the world by medical missionaries, and the dissemination of textbooks. Japanese elites enthusiastically embraced Western medicine after the Meiji Restoration of the 1860s. However they had been prepared by their knowledge of the Dutch and German medicine, for they had some contact with Europe through the Dutch. Highly influential was the 1765 edition of Hendrik van Deventer's pioneer work Nieuw Ligt ("A New Light") on Japanese obstetrics, especially on Katakura Kakuryo's publication in 1799 of Sanka Hatsumo ("Enlightenment of Obstetrics").
A cadre of Japanese physicians began to interact with Dutch doctors, who introduced smallpox vaccinations. By 1820 Japanese ranpô medical practitioners not only translated Dutch medical texts, they integrated their readings with clinical diagnoses. These men became leaders of the modernization of medicine in their country. They broke from Japanese traditions of closed medical fraternities and adopted the European approach of an open community of collaboration based on expertise in the latest scientific methods.
Kitasato Shibasaburō (1853-1931) studied bacteriology in Germany under Robert Koch. In 1891 he founded the Institute of Infectious Diseases in Tokyo, which introduced the study of bacteriology to Japan. He and French researcher Alexandre Yersin went to Hong Kong in 1894, where; Kitasato confirmed Yersin's discovery that the bacterium Yersinia pestis is the agent of the plague. In 1897 he isolates and described the organism that caused dysentery. He became the first dean of medicine at Keio University, and the first president of the Japan Medical Association.
Japanese physicians immediately recognized the values of X-Rays. They were able to purchase the equipment locally from the Shimadzu Company, which developed, manufactured, marketed, and distributed X-Ray machines after 1900. Japan not only adopted German methods of public health in the home islands, but implemented them in its colonies, especially Korea and Taiwan, and after 1931 in Manchuria. A heavy investment in sanitation resulted in a dramatic increase of life life expectancy.
The Quaker-run York Retreat, founded in 1796, gained international prominence as a centre for moral treatment and a model of asylum reform following the publication of Samuel Tuke's Description of the Retreat (1813)
Until the nineteenth century, the care of the insane was largely a communal and family responsibility rather than a medical one. The vast majority of the mentally ill were treated in domestic contexts with only the most unmanageable or burdensome likely to be institutionally confined. This situation was transformed radically from the late eighteenth century as, amid changing cultural conceptions of madness, a new-found optimism in the curability of insanity within the asylum setting emerged. Increasingly, lunacy was perceived less as a physiological condition than as a mental and moral one to which the correct response was persuasion, aimed at inculcating internal restraint, rather than external coercion. This new therapeutic sensibility, referred to as moral treatment, was epitomised in French physician Philippe Pinel's quasi-mythological unchaining of the lunatics of the Bicêtre Hospital in Paris and realised in an institutional setting with the foundation in 1796 of the Quaker-run York Retreat in England.

Patient, Surrey County Lunatic Asylum, c. 1850–58. The asylum population in England and Wales rose from 1,027 in 1827 to 74,004 in 1900
From the early nineteenth century, as lay-led lunacy reform movements gained in influence, ever more state governments in the West extended their authority and responsibility over the mentally ill. Small-scale asylums, conceived as instruments to reshape both the mind and behaviour of the disturbed, proliferated across these regions. By the 1830s, moral treatment, together with the asylum itself, became increasingly medicalised and asylum doctors began to establish a distinct medical identity with the establishment in the 1840s of associations for their members in France, Germany, the United Kingdom and America, together with the founding of medico-psychological journals.
Medical optimism in the capacity of the asylum to cure insanity soured by the close of the nineteenth century as the growth of the asylum population far outstripped that of the general population.[a] Processes of long-term institutional segregation, allowing for the psychiatric conceptualisation of the natural course of mental illness, supported the perspective that the insane were a distinct population, subject to mental pathologies stemming from specific medical causes. As degeneration theory grew in influence from the mid-nineteenth century, heredity was seen as the central causal element in chronic mental illness, and, with national asylum systems overcrowded and insanity apparently undergoing an inexorable rise, the focus of psychiatric therapeutics shifted from a concern with treating the individual to maintaining the racial and biological health of national populations.
Emil Kraepelin (1856–1926) introduced new medical categories of mental illness, which eventually came into psychiatric usage despite their basis in behavior rather than pathology or etiology. Shell shock among frontline soldiers exposed to heavy artillery bombardment was first diagnosed by British Army doctors in 1915. By 1916, similar symptoms were also noted in soldiers not exposed to explosive shocks, leading to questions as to whether the disorder was physical or psychiatric.In the 1920s surrealist opposition to psychiatry was expressed in a number of surrealist publications. In the 1930s several controversial medical practices were introduced including inducing seizures (by electroshock, insulin or other drugs) or cutting parts of the brain apart (leucotomy or lobotomy). Both came into widespread use by psychiatry, but there were grave concerns and much opposition on grounds of basic morality, harmful effects, or misuse.
In the 1950s new psychiatric drugs, notably the antipsychotic chlorpromazine, were designed in laboratories and slowly came into preferred use. Although often accepted as an advance in some ways, there was some opposition, due to serious adverse effects such as tardive dyskinesia. Patients often opposed psychiatry and refused or stopped taking the drugs when not subject to psychiatric control. There was also increasing opposition to the use of psychiatric hospitals, and attempts to move people back into the community on a collaborative user-led group approach ("therapeutic communities") not controlled by psychiatry. Campaigns against masturbation were done in the Victorian era and elsewhere. Lobotomy was used until the 1970s to treat schizophrenia. This was denounced by the anti-psychiatric movement in the 1960s and later.
REFERENCE:
http://en.wikipedia.org/wiki/History_of_medicine